Cannabis, Neuroprotection and Traumatic Brain Injuries
All Blog PostsFor millennia, cannabis was revered as a medicinal substance until recent decades, where it has been unjustly vilified as a substance of abuse. However, thanks to the relentless pursuit of knowledge by many brilliant researchers across the world, it is now recognized for its profound interaction with a crucial physiological system known as the endocannabinoid system (ECS). This intricate network, pervasive throughout our brains and bodies, diligently maintains internal balance, or homeostasis.
The ECS came into focus during investigations into the effects of THC, the primary psychoactive component of cannabis. Operating akin to a sophisticated lock-and-key mechanism, cannabinoid receptors serve as the locks embedded within cell membranes. These receptors are activated by various chemical compounds, including endocannabinoids produced internally, phytocannabinoids from the cannabis plant, and synthetic cannabinoids crafted for research purposes. When a cannabinoid binds to its respective receptor, it triggers a cascade of chemical signals within the cell, prompting alterations in cellular communication. For example, individuals experiencing pain may find relief through cannabis use, as cannabinoids modify the perception of pain by influencing cannabinoid receptors in brain cells, thereby dampening the transmission of pain signals.
Understanding the distribution of cannabinoid receptors enables us to grasp the diverse conditions that cannabinoid-based medicines can potentially address. In the brain, these receptors are situated in regions governing pain, nausea, learning, stress response, memory, appetite, motor coordination, and higher cognitive functions. Similarly, in the body, cannabinoid receptors predominantly reside in the gut, immune system, and liver, as well as many other organs and tissues, playing significant roles in regulating inflammation.
Traumatic brain injuries (TBIs) induce primary damage upon impact, followed by a cascade of secondary mechanisms that cause further harm to the brain. Injured neurons release glutamate, a neurotransmitter that becomes toxic when accumulated. This glutamate surplus triggers a series of chemical reactions intensifying brain damage. Moreover, TBIs prompt the release of vasoconstrictive chemicals, reducing blood flow and resulting in energy deprivation and cell damage and death. Concurrently, brain inflammation ensues rapidly post-injury, compounding the destruction of brain cells. This multifaceted assault on brain tissue underscores the difficult challenge in treating TBIs, requiring interventions addressing various pathological processes simultaneously.
Fortunately, the body activates innate protective mechanisms following TBI to mitigate damage and restore equilibrium. Research indicates that the ECS springs into action immediately after an injury, with endocannabinoids impeding the release of compounds that aggravate secondary brain damage. Furthermore, endocannabinoids exhibit anti-inflammatory and antioxidant properties, fostering brain cell survival post-injury.
Given the similarities between synthetic and plant-derived cannabinoids and endocannabinoids, researchers have explored their potential neuroprotective effects in TBI. Encouragingly, studies demonstrate that synthetic cannabinoids shield against brain cell damage in animal models of brain injury. Cannabidiol (CBD), administered promptly following oxygen and blood flow interruption, has shown promise in reducing brain cell injury, swelling, seizures, and motor impairment. CBD has also been found to promote neurogenesis - the process by which new neurons are formed in the brain - through multiple mechanisms including increased receptor signaling to regulate stem cell proliferation and differentiation in the hippocampus. Additionally, CBD enhances endocannabinoids by inhibiting their breakdown, thereby augmenting self-neuroprotective mechanisms. CBD also increases brain-derived neurotrophic factor (BDNF), an important neurotrophin involved in the recovery process from TBI. Another mechanism by which CBD is neuroprotective is through the suppression of blood brain barrier (BBB) permeability, which is a consequence of brain injury. Other cannabinods appear to be neuroprotective as well. Notably, THC has been linked to reduced glutamate release in animals with brain injuries, while clinical data suggests a lower risk of death among TBI patients testing positive for THC. In a preclinical trial, cannabigerol (CBG) and cannabidivarin (CBDV) were protective against injury to three different cells that constitute the BBB.
TBI patients should not endure prolonged suffering when the neuroprotective, antioxidant, and anti-inflammatory properties of cannabinoid compounds appear to mitigate and possibly prevent the dire consequences of brain injury. It is essential for researchers and clinicians to have the freedom to explore cannabis compounds in the treatment of TBI and brain injury, facilitating early interventions that may offer hope for these patients.
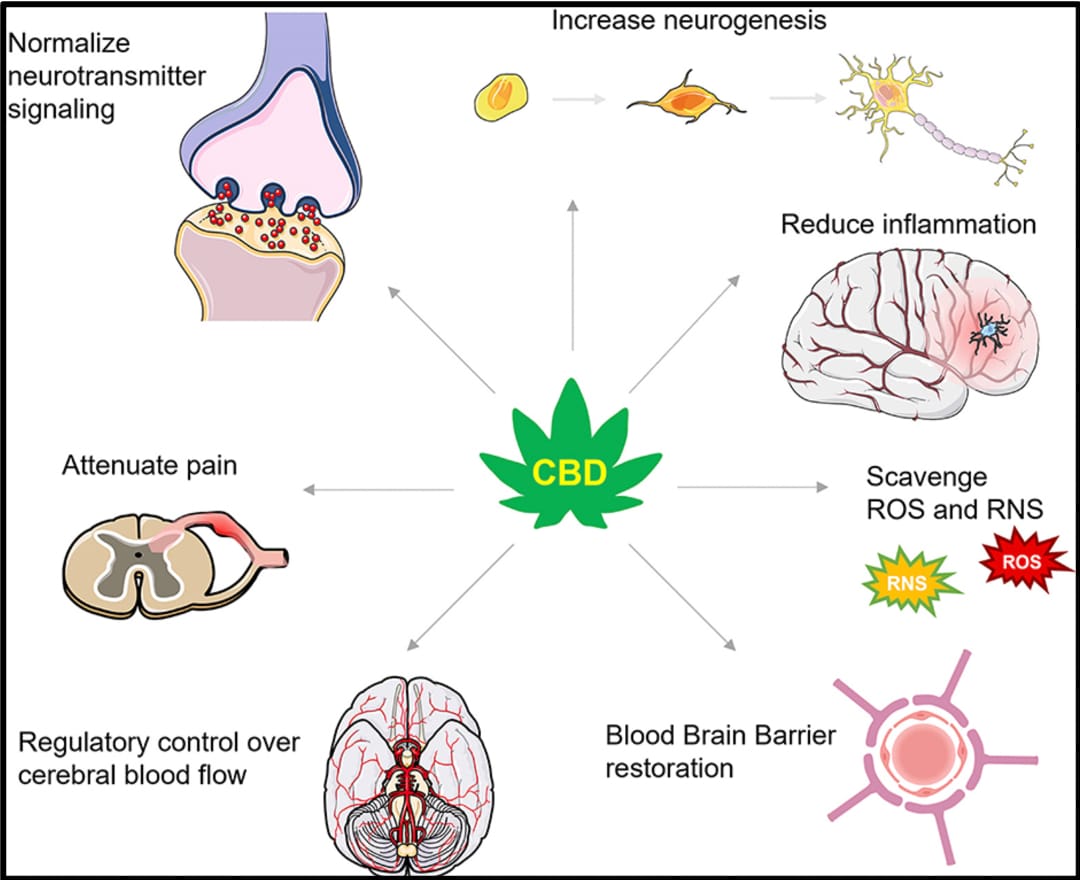
IMAGE SOURCE: Aychman, Mackenzie M., David L. Goldman, and Joshua S. Kaplan. "Cannabidiol's neuroprotective properties and potential treatment of traumatic brain injuries." Frontiers in neurology 14 (2023): 1087011.